Question What are the trends of utilization and spending on brand-name and generic formulations of low-density lipoprotein cholesterol (LDL-C)–lowering therapies among Medicare beneficiaries between 2014 and 2018?
Findings In this cross-sectional study of the Medicare Part D database, between 2014 and 2018, prescription of LDL-C–lowering therapies increased 23% while total expenditures decreased 46% among Medicare beneficiaries, largely driven by greater use of generic statin formulations. PCSK9 inhibitor use and spending increased 144% and 199%, respectively, over the study period; an additional $2.5 billion could have been saved if generic substitution occurred once available.
Meaning Medicare expenditures on LDL-C–lowering therapy have declined despite increasing use driven by rapid and sustained uptake of generic formulations; however, further work is needed to ensure cost does not become a barrier to care.
Importance Low-density lipoprotein cholesterol (LDL-C)–lowering therapies are a cornerstone of prevention in atherosclerotic cardiovascular disease. With the introduction of generic formulations and the release of new therapies, including proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, contemporary Medicare utilization of these therapies remains unknown.
Objective To determine trends in utilization and spending on brand-name and generic LDL-C–lowering therapies and to estimate potential savings if all Medicare beneficiaries were switched to available therapeutically equivalent generic formulations.
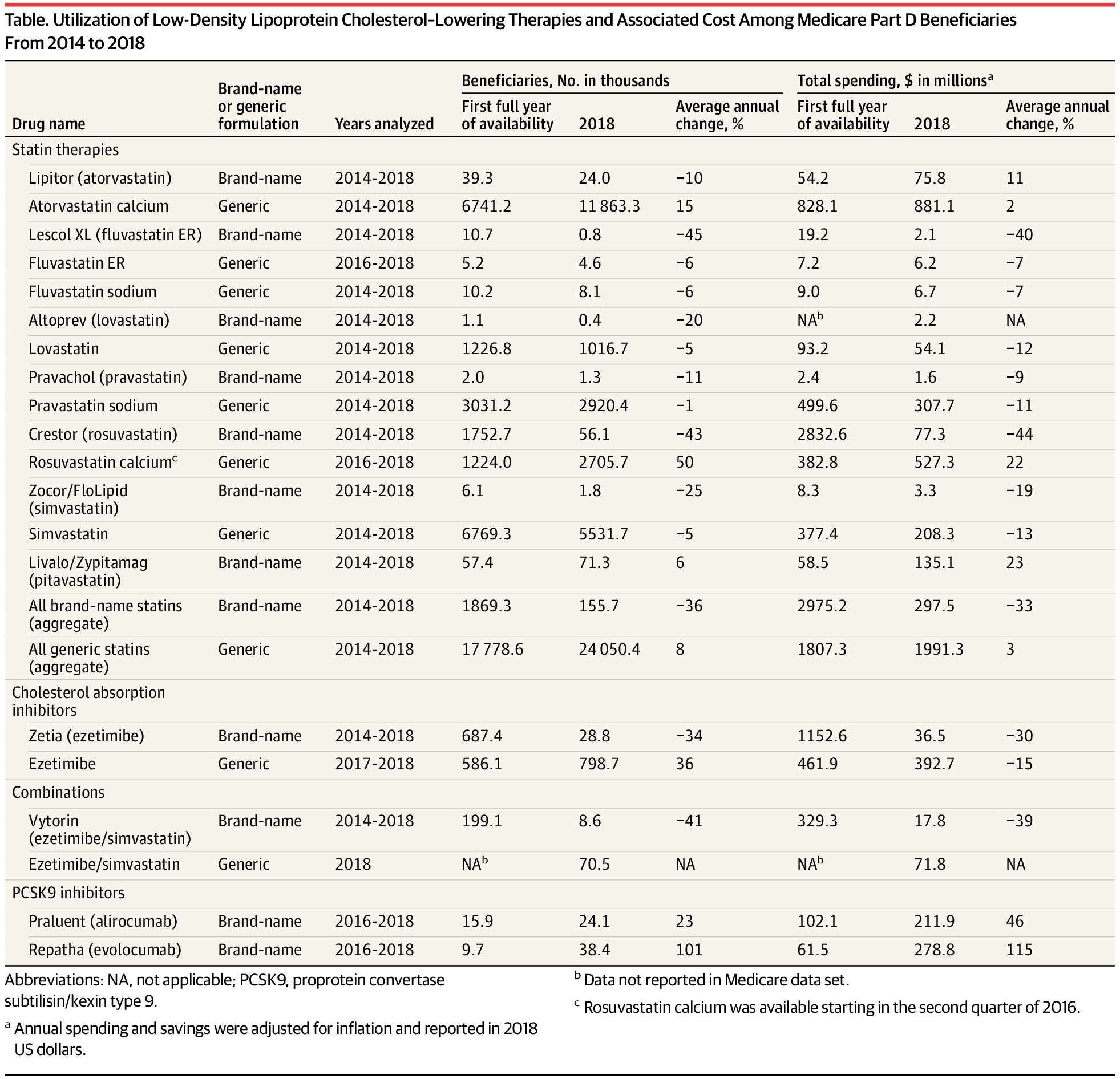
Design, Setting, and Participants This cross-sectional study analyzed prescription drug utilization and cost trend data from the Medicare Part D Prescription Drug Event data set from 2014 to 2018 for LDL-C–lowering therapies. A total of 11 LDL-C–lowering drugs with 25 formulations, including 16 brand-name and 9 generic formulations, were included. Data were collected and analyzed from October 2019 to June 2020.
Main Outcomes and Measures Number of Medicare Part D beneficiaries, annual spending, and spending per beneficiary for all formulations.
Results The total number of Medicare Part D beneficiaries ranged from 37 720 840 in 2014 to 44 249 461 in 2018. The number of Medicare beneficiaries taking LDL-C–lowering therapies increased by 23% (from 20.5 million in 2014 to 25.2 million in 2018), while the associated Medicare expenditure decreased by 46% (from $6.3 billion in 2014 to $3.3 billion in 2018). Lower expenditure was driven by greater uptake of generic statin and ezetimibe and a concurrent rapid decline in the use of their brand-name formulations. Medicare spent $9.6 billion on brand-name statins and ezetimibe and could have saved $2.1 billion and $0.4 billion, respectively, if brand-name formulations were switched to equivalent generic versions when available. The number of beneficiaries using PCSK9 inhibitors since their introduction in 2015 has been modest, although use has increased by 144% (from 25 569 in 2016 to 62 476 in 2018) and total spending has increased by 199% (from $164 million in 2016 to $491 million in 2018).
Conclusions and Relevance Between 2014 and 2018, LDL-C–lowering therapies were used by 4.8 million more Medicare beneficiaries annually, with an associated $3.0 billion decline in Medicare spending. This cost reduction was driven by the rapid transition from brand-name formulations to lower-cost generic formulations of statins and ezetimibe. Use of PCSK9 inhibitions, although low, increased over time and could have broad implications on future Medicare spending.
KIMB00P on September 9th, 2020 at 22:36 UTC »
It’s also because once a generic is available, insurances will begin to deny coverage for brand name drugs. They will require a prior authorization requesting info on why the patient can’t take the cheaper generic option.
Pharmacy technician.
ryanj72 on September 9th, 2020 at 20:56 UTC »
For anyone reading comments, looking for ways to personally save money on prescriptions, I cannot recommend GoodRx enough. Even if you have insurance, check their website first to see if you can get a better deal. Twice in the past month, my wife, who is insured here in the U.S., found it much cheaper to pay cash out of pocket and not using her insurance. One drug was $156 USD with her insurance. We checked GoodRx, found a coupon that ended up being $28 USD for the exact same prescription. For any US citizens, it's best to check the website, and then check the pharmacy to see if it's cheaper using your insurance or without.
It makes no sense why it would be cheaper to pay out of pocket with a coupon, then to use your own insurance. And you wonder why health insurance companies are making record breaking profits....
TheKingofHearts26 on September 9th, 2020 at 18:20 UTC »
Yes this is standard practice, and not just for Medicare patients. There’s rarely a time when the brand name should be used over an available generic. And it’s no secret that generics cost less since they can benefit from the research out in by other groups without the cost investment.