New research has found that neurons deep inside the brain could hold the key to accurately diagnosing bipolar disorder and depression.
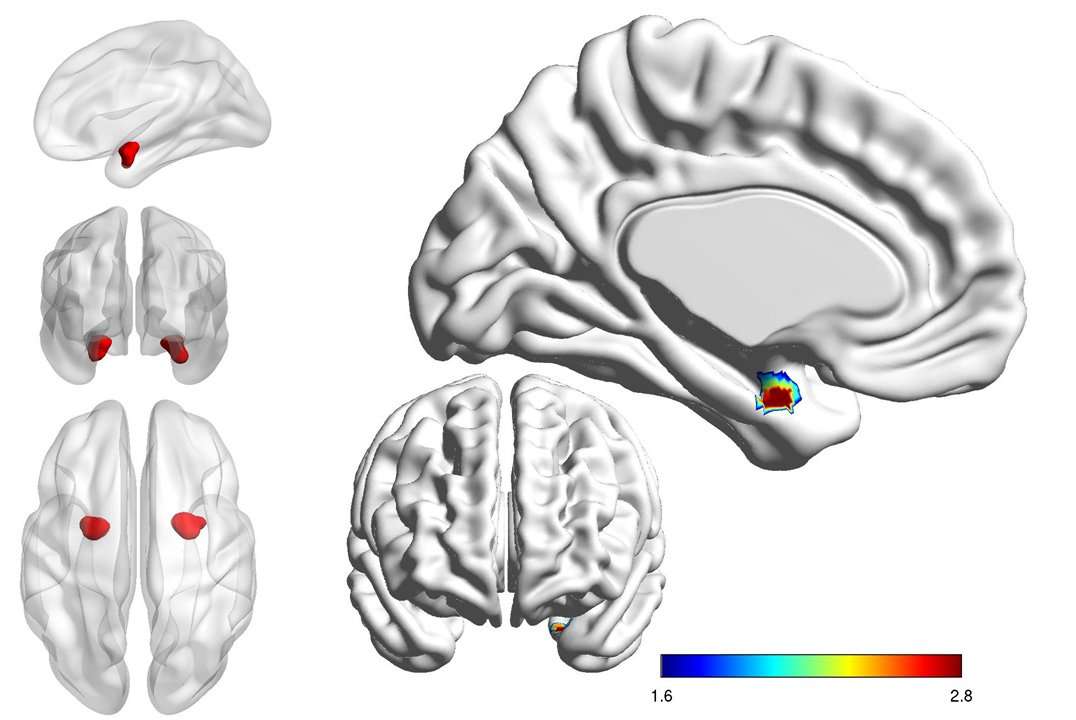
The research team used sophisticated MRI scanning to see how the amygdala – a set of neurons that play a key role in processing emotions – reacts as a patient processes facial expressions such as anger, fear, sadness, disgust and happiness.
The research showed that this key structure within the brain responds differently depending on whether the person has bipolar disorder or depression.
In people with bipolar disorder, the left side of the amygdala is less active and less connected with other parts of the brain than in people with depression.
The findings from this study had 80% accuracy in making this distinction.
Lead researcher Dr Mayuresh Korgaonkar from the Westmead Institute for Medical Research and the University of Sydney said these differences could potentially be used in the future to differentiate bipolar disorder from depressive disorders.
“Mental illness, particularly bipolar disorder and depression, can be difficult to diagnose as many conditions have similar symptoms,” Dr Korgaonkar said.
“These two illness are virtually identical except that in bipolar individuals also experience mania.
“This means distinguishing them can be difficult and presents a major clinical challenge as treatment varies considerably depending on the primary diagnosis.
“The wrong diagnosis can be dangerous, leading to poor social and economic outcomes for the patient as they undergo treatment for a completely different disorder.
Identifying brain markers that could reliably tell bipolar disorder and depression apart would have immense clinical benefit.
“Such a marker could help us better understand both these disorders, identify risk factors for developing these disorders, and potentially enable clear diagnosis from early onset,” Dr Korgaonkar said.
Approximately 60% of patients with bipolar disorder are initially misdiagnosed as major depressive disorder.
Alarming, it can take up to a decade for these patients to be accurately diagnosed with bipolar disorder.
Bipolar disorder often first presents in the depressive phase of the illness and bipolar depression is similar to major depression in terms of clinical symptoms.
Emotion processing is a core problem underlying both these disorders.
Dr Korgaonkar and his team are now running phase 2 of this study, which aims to further characterise these identified markers in a larger cohort of patients.
People interested in participating in phase 2 of the study, or who would like further information, should contact Wendy Chen on 02 8627 3306 or [email protected].
Learn more about phase 2 of the study: Biomarkers to differentiate bipolar from unipolar depression.
The research paper has been published in a leading international scientific journal Biological Psychiatry: Cognitive Neuroscience and NeuroImaging https://www.sciencedirect.com/science/article/pii/S2451902218302362.
The National Health and Medical Research Council (NHMRC) funded this study.
The study was led by the Westmead Institute of Medical Research and the University of Sydney, and completed in collaboration with colleagues from Westmead Hospital, Royal North Shore Hospital and Stanford University.
capybarometer on September 9th, 2018 at 11:58 UTC »
Being able to diagnose mental illness with a brain scan could conceivably save significant time and money and reduce suffering. Like the study says, an individual in a depressive episode can often look the same regardless of etiology, but one problem not mentioned is that giving someone with bipolar depression commonly used antidepressants can often make that person manic. Right now, this is sometimes unavoidable, as a person who has never experienced a manic or hypomanic episode cannot convey this information. Even worse, inpatient psychiatric hospitals often have to clean up the messes created by psychiatrists who get a sloppy history from someone and miss obvious signs of past manic or hypomanic episodes, which is expensive and prevents patients from living their lives for days, if not weeks.
lampishthing on September 9th, 2018 at 11:34 UTC »
I often wonder in cases like these if the research was closer to 100% accurate in diagnosing a disorder but the illness that we have defined is an inaccurate description physiologically or simply overbroad.
mvea on September 9th, 2018 at 10:39 UTC »
The title of the post is a copy and paste from the second, fifth and seventh paragraphs of the linked academic press release here :
Journal Reference:
Mayuresh S. Korgaonkar, May Erlinger, Isabella A. Breukelaar, Philip Boyce, Philip Hazell, Cassandra Antees, Sheryl Foster, Stuart M. Grieve, Lavier Gomes, Leanne M. Williams, Anthony W.F. Harris, Gin S. Malhi,
Amygdala activation and connectivity to emotional processing distinguishes asymptomatic patients with bipolar disorders and unipolar depression,
Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 2018, ISSN 2451-9022,
Doi: https://doi.org/10.1016/j.bpsc.2018.08.012.
Link: http://www.sciencedirect.com/science/article/pii/S2451902218302362
Abstract:
Background
Mechanistically based neural markers such as amygdala reactivity offer one approach to addressing the challenges of differentiating bipolar and unipolar depressive disorders, independently from mood state and acute symptoms. Although emotion-elicited amygdala reactivity has been found to distinguish bipolar from unipolar patients in depressed states, it remains unknown whether this distinction is trait-like and present in the absence of an acutely depressed mood. We address this gap by investigating bipolar (BP) and unipolar major depressive disorder (MDD) populations in remission.
Methods
73 participants (23 BP and 25 MDD patients matched for age-gender, number of depressive episodes and severity; 25 age-gender matched healthy individuals) completed supra- and subliminal processing of threat, sad, happy and neutral faces during fMRI. We compared groups for activation and connectivity for the amygdala.
Results
BP participants had lower left amygdala activation than MDD during supraliminal and subliminal threat, sad and neutral processing and for subliminal happy faces. BP participants also exhibited lower amygdala connectivity to the insula and hippocampus for threat and to medial orbito-frontal for happy supraliminal and subliminal processing. BP participants also demonstrated greater amygdala-insula connectivity for sad supraliminal and subliminal face processing. Both patient groups were distinct from controls across several measures for activation and connectivity.
Conclusion
Independent of valence or level of emotional awareness amygdala activation and connectivity during facial emotion processing can distinguish BP and MDD patients. These findings provide evidence that this neural substrate could be a potential trait-marker to differentiate these two disorders largely independent of illness state.