Question Do any of 4 oral combination analgesics (3 with different opioids and 1 opioid-free) provide more effective reduction of moderate to severe acute extremity pain in the emergency department (ED)?
Findings In this randomized clinical trial of 411 ED patients with acute extremity pain (mean score, 8.7 on the 11-point numerical rating scale), there was no significant difference in pain reduction at 2 hours. Mean pain scores decreased by 4.3 with ibuprofen and acetaminophen (paracetamol); 4.4 with oxycodone and acetaminophen; 3.5 with hydrocodone and acetaminophen; and 3.9 with codeine and acetaminophen.
Meaning For adult ED patients with acute extremity pain, there were no clinically important differences in pain reduction at 2 hours with ibuprofen and acetaminophen or 3 different opioid and acetaminophen combination analgesics.
Importance The choice of analgesic to treat acute pain in the emergency department (ED) lacks a clear evidence base. The combination of ibuprofen and acetaminophen (paracetamol) may represent a viable nonopioid alternative.
Objectives To compare the efficacy of 4 oral analgesics.
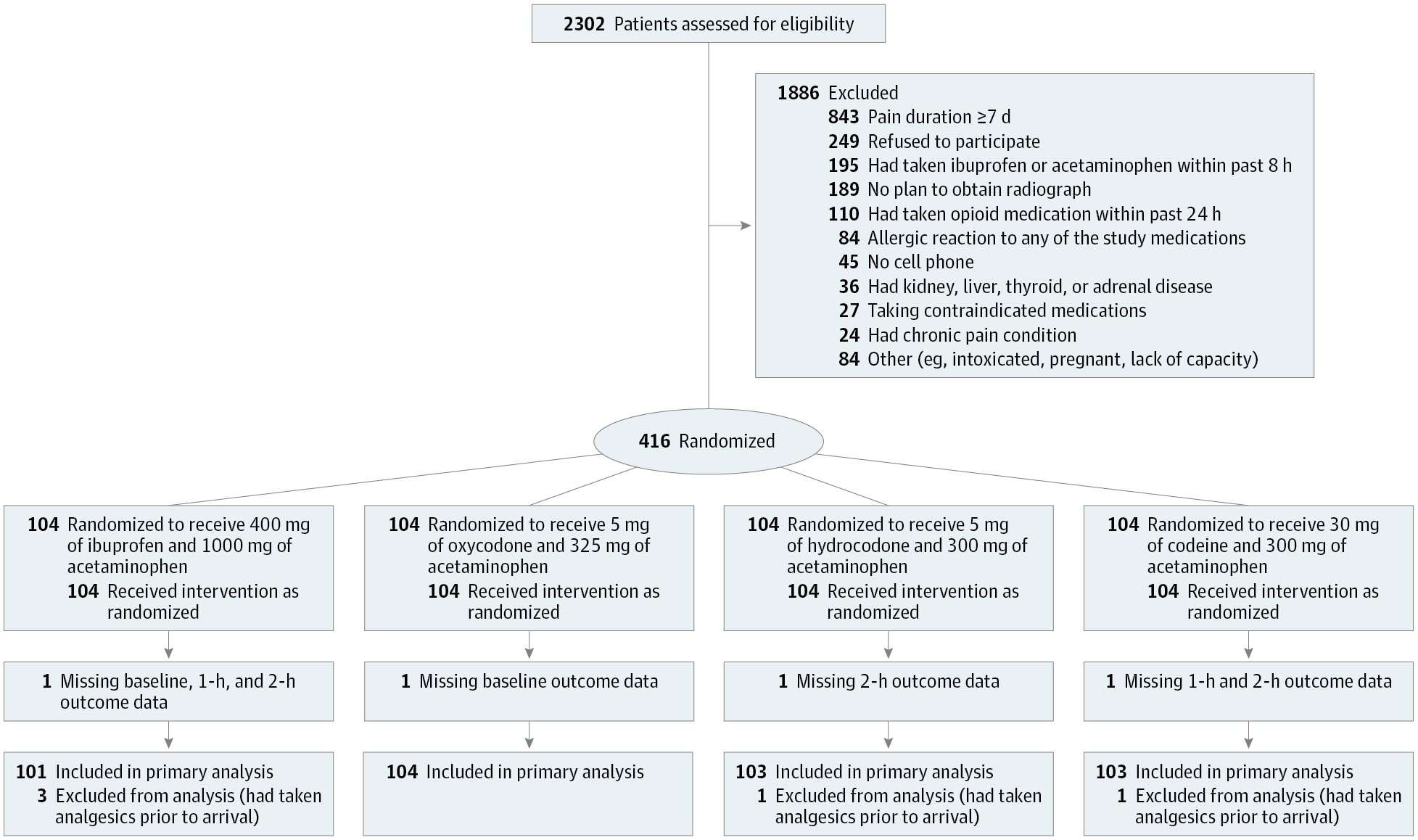
Design, Settings, and Participants Randomized clinical trial conducted at 2 urban EDs in the Bronx, New York, that included 416 patients aged 21 to 64 years with moderate to severe acute extremity pain enrolled from July 2015 to August 2016.
Interventions Participants (104 per each combination analgesic group) received 400 mg of ibuprofen and 1000 mg of acetaminophen; 5 mg of oxycodone and 325 mg of acetaminophen; 5 mg of hydrocodone and 300 mg of acetaminophen; or 30 mg of codeine and 300 mg of acetaminophen.
Main Outcomes and Measures The primary outcome was the between-group difference in decline in pain 2 hours after ingestion. Pain intensity was assessed using an 11-point numerical rating scale (NRS), in which 0 indicates no pain and 10 indicates the worst possible pain. The predefined minimum clinically important difference was 1.3 on the NRS. Analysis of variance was used to test the overall between-group difference at P = .05 and 99.2% CIs adjusted for multiple pairwise comparisons.
Results Of 416 patients randomized, 411 were analyzed (mean [SD] age, 37 [12] years; 199 [48%] women; 247 [60%] Latino). The baseline mean NRS pain score was 8.7 (SD, 1.3). At 2 hours, the mean NRS pain score decreased by 4.3 (95% CI, 3.6 to 4.9) in the ibuprofen and acetaminophen group; by 4.4 (95% CI, 3.7 to 5.0) in the oxycodone and acetaminophen group; by 3.5 (95% CI, 2.9 to 4.2) in the hydrocodone and acetaminophen group; and by 3.9 (95% CI, 3.2 to 4.5) in the codeine and acetaminophen group (P = .053). The largest difference in decline in the NRS pain score from baseline to 2 hours was between the oxycodone and acetaminophen group and the hydrocodone and acetaminophen group (0.9; 99.2% CI, −0.1 to 1.8), which was less than the minimum clinically important difference in NRS pain score of 1.3. Adverse events were not assessed.
Conclusions and Relevance For patients presenting to the ED with acute extremity pain, there were no statistically significant or clinically important differences in pain reduction at 2 hours among single-dose treatment with ibuprofen and acetaminophen or with 3 different opioid and acetaminophen combination analgesics. Further research to assess adverse events and other dosing may be warranted.
digitallimit on November 8th, 2017 at 03:41 UTC »
Ibuprofen and Acetaminophen respectively for the brand averse.
Dannysmartful on November 8th, 2017 at 03:31 UTC »
Years ago my pharmacist recommended taking 2 Tylenol and 2 Advil together because they will not interact with each other -one is a pain blocker and the other is an anti-inflammatory.
Now if I ever have very severe pain I take them together and the pain goes away. This has been very beneficial because strong pain medications cause me to vomit or blackout so I always avoid them.
Bisnono on November 8th, 2017 at 03:00 UTC »
It's an interesting study, although it could also be indicative of overprescribing of opioids when they simply aren't warranted for that type of injury rather than reflecting the equality of medication effectiveness for pain management. I'd be more convinced if this were a study of patients experiencing pain from nerve damage, cancer, surgery post-op, or kidney stones. Also, the fact that 20% of patients still needed additional pain medication is not insignificant.