Of all the kinds of bacteria, some are charming and beneficial, others are malicious and dangerous—and then there are the ones that are just plain turds.
That’s the case for Mycoplasma hyorhinis and its ilk.
Researchers caught the little jerks hiding out among cancer cells, gobbling up chemotherapy drugs intended to demolish their tumorous digs. The findings, reported this week in Science, explain how some otherwise treatable cancers can thwart powerful therapies.
Drug resistance among cancers is a “foremost challenge,” according to the study’s authors, led by Ravid Straussman at the Weizmann Institute of Science. Yet the new data suggest that certain types of drug-resistant cancers could be defeated with a simple dollop of antibiotics alongside a chemotherapy regimen.
That said, the findings are still mostly from lab and animal experiments. It will be a while before the results are repeated and confirmed in human cancer cases, then possibly translated into new clinical practices for treating certain types and cases of cancers.
Dr. Straussman and his colleagues got a hunch to look for the bacteria after noticing that, when they grew certain types of human cancer cells together in lab, the cells all became more resistant to a chemotherapy drug called gemcitabine. This is a drug used to treat pancreatic, lung, breast, and bladder cancers and is often sold under the brand name Gemzar.
The researchers suspected that some of the cells may secrete a drug-busting molecule. So they tried filtering the cell cultures to see if they could catch it. Instead, they found that the cells lost their resistance after being passed through a pretty large filter—0.45 micrometers. This would catch large particles—like bacteria—but not small molecules, as the researchers were expecting.
Looking closer, the researchers noticed that some of their cancer cells were contaminated with M. hyorhinis. And these bacteria could metabolize gemcitabine, rendering the drug useless. When the researchers transplanted treatable cancer cells into the flanks of mice—some with and some without M. hyorhinis—the bacteria-toting tumors were resistant to gemcitabine treatment.
And it’s not just M. hyorhinis that can turn tumors resistant. When the researchers pinpointed the gene that encodes the molecular machinery for disarming gemcitabine in M. hyorhinis—a gene called CDD L —they found that it’s quite common in other bacteria. In initial testing of 27 bacterial species, 13 could knock out gemcitabine. When the researchers searched through the genetics of nearly 2,700 bacteria, they found that hundreds also had the gene for defeating gemcitabine. Most of those bacteria were in the Gammaproteobacteria class, a giant group of bacteria that includes E. coli and Salmonella.
To see if this may be a real problem in humans, the researchers gathered 113 cell samples from human pancreatic cancers (a cancer type called pancreatic ductal adenocarcinoma). These were all collected during cancer surgeries. The researchers also assembled 20 samples from organ donors that had non-cancerous pancreases (or “pancreata,” if we're being persnickety). Of the 113 cancer samples, 86 had signs of bacteria present—mostly Gammaproteobacteria—while only three of the 20 non-cancerous samples had bacteria.
The researchers speculate that bacteria may invade pancreatic tumors by migrating from the duodenum, the top section of the small intestine.
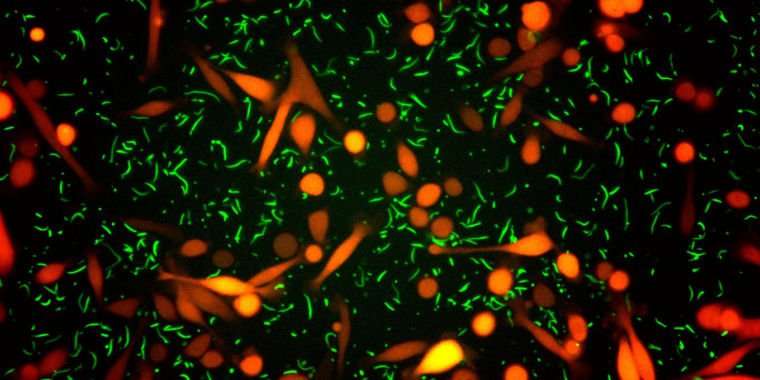
To put all their findings together, the researchers engineered an E. coli strain to carry CDD L —a gene it didn’t carry before—then injected the strain into tumor-riddled mice. The researchers used fluorescent markers to track both the bacteria and the tumors. When they treated the mice with either gemcitabine and an antibiotic or just gemcitabine alone, they saw bacteria disappear and tumors shrink in the mice that got the antibiotic-chemotherapy combo. But in the mice with just chemotherapy, the researches saw rapid tumor progression.
The role of bacteria in drug-resistant cancers and the potential for using antibiotics with chemotherapies “merit additional exploration,” the authors conclude.
Science, 2017. DOI: 10.1126/science.aah5043 (About DOIs).
carbonclasssix on September 18th, 2017 at 14:17 UTC »
This is really interesting, but wouldn't cytidine deaminase be expressed in the cancer cells as well? I would think a pyrimidine scavenging enzyme would be present in most if not all cells. Maybe it's something unique to the bacterial version, or cancer cells don't express this gene?
SirT6 on September 18th, 2017 at 13:53 UTC »
Seems like this is a fun example of serendipity and being able to think outside the box leading to a Science paper. Reading between the lines, it seems like they had no a priori hypothesis that suggested that bacteria may mediate chemo-resistance in their models. Rather, it looks like they had a mycoplasma infection in their cells, and instead of scrapping everything (which is the most common response), they dug in and got a high impact publication out of it.
That said, I am a bit skeptical about the big picture link between bacteria and chemo-resistance. The phenotype they described was initially reported in cell culture (warm, dark environment that favors bacterial growth), and followed up in a mouse model where they injected millions of tumor-targeting bacteria into mice.
I would have loved to see some more human data because I am struggling to get on board with the idea that there are sufficient numbers of bacteria in the tumor environment to actually modify the chemo to an inert compound. For example, do PDX samples from patient's high in bacteria exhibit higher chemo-resistance? Or if you look at the TCGA database, can you find people who have higher numbers of bacterial DNA also have poorer survival outcomes?
mvea on September 18th, 2017 at 13:03 UTC »
Journal reference:
Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine
Leore T. Geller1,, Michal Barzily-Rokni2,, Tal Danino3,†, Oliver H. Jonas4,5, Noam Shental6, Deborah Nejman1, Nancy Gavert1, Yaara Zwang1, Zachary A. Cooper7,8,‡, Kevin Shee2, Christoph A. Thaiss9, Alexandre Reuben8, Jonathan Livny2, Roi Avraham10, Dennie T. Frederick11, Matteo Ligorio12, Kelly Chatman13, Stephen E. Johnston2, Carrie M. Mosher2, Alexander Brandis14, Garold Fuks15, Candice Gurbatri16, Vancheswaran Gopalakrishnan8, Michael Kim8, Mark W. Hurd17, Matthew Katz8, Jason Fleming8, Anirban Maitra18, David A. Smith2, Matt Skalak3, Jeffrey Bu3, Monia Michaud19, Sunia A. Trauger13, Iris Barshack20,21, Talia Golan21,22, Judith Sandbank21, Keith T. Flaherty12, Anna Mandinova2,23, Wendy S. Garrett2,19,24, Sarah P. Thayer25, Cristina R. Ferrone26, Curtis Huttenhower2,27, Sangeeta N. Bhatia2,28,29,30,31,32,33, Dirk Gevers2,§, Jennifer A. Wargo7,8, Todd R. Golub34,35,36,∥, Ravid Straussman1,∥,¶
Science 15 Sep 2017: Vol. 357, Issue 6356, pp. 1156-1160 DOI: 10.1126/science.aah5043
Link: http://science.sciencemag.org/content/357/6356/1156
Debugging a cancer therapy
Abstract