In December 2020, the US Food and Drug Administration (FDA) issued Emergency Use Authorizations for 2 mRNA-based vaccines for prevention of coronavirus disease 2019 (COVID-19): Pfizer-BioNTech COVID-19 vaccine (EUA issued December 11; 2 doses, 3 weeks apart) and Moderna COVID-19 vaccine (EUA issued December 18; 2 doses, 1 month apart). Shortly after each authorization, the Advisory Committee on Immunization Practices issued interim recommendations for use.1,2
Following implementation of vaccination, cases of anaphylaxis after administration of the Pfizer-BioNTech and Moderna vaccines began to be reported.3,4 Anaphylaxis is a life-threatening allergic reaction that can occur after vaccination, with onset typically within minutes to hours.5 The initial estimated reporting rates for anaphylaxis in the US were 11.1 cases per million doses administered of the Pfizer-BioNTech vaccine (December 14-23, 2020) and 2.5 cases per million doses administered of the Moderna vaccine (December 21, 2020-January 10, 2021).3,4 Since these early estimates were generated, millions more doses of both vaccines have been administered and safety monitoring has detected additional cases of anaphylaxis. This analysis updates the reporting rates of anaphylaxis in individuals following receipt of either the Pfizer-BioNTech or Moderna vaccine.
The Vaccine Adverse Event Reporting System (VAERS), the national passive surveillance (spontaneous reporting) system for adverse events after immunization,6 captured notifications and reports of suspected anaphylaxis following vaccination. Physicians at the Centers for Disease Control and Prevention (CDC) evaluated these reports and applied the Brighton Collaboration case definition for anaphylaxis to classify cases.7
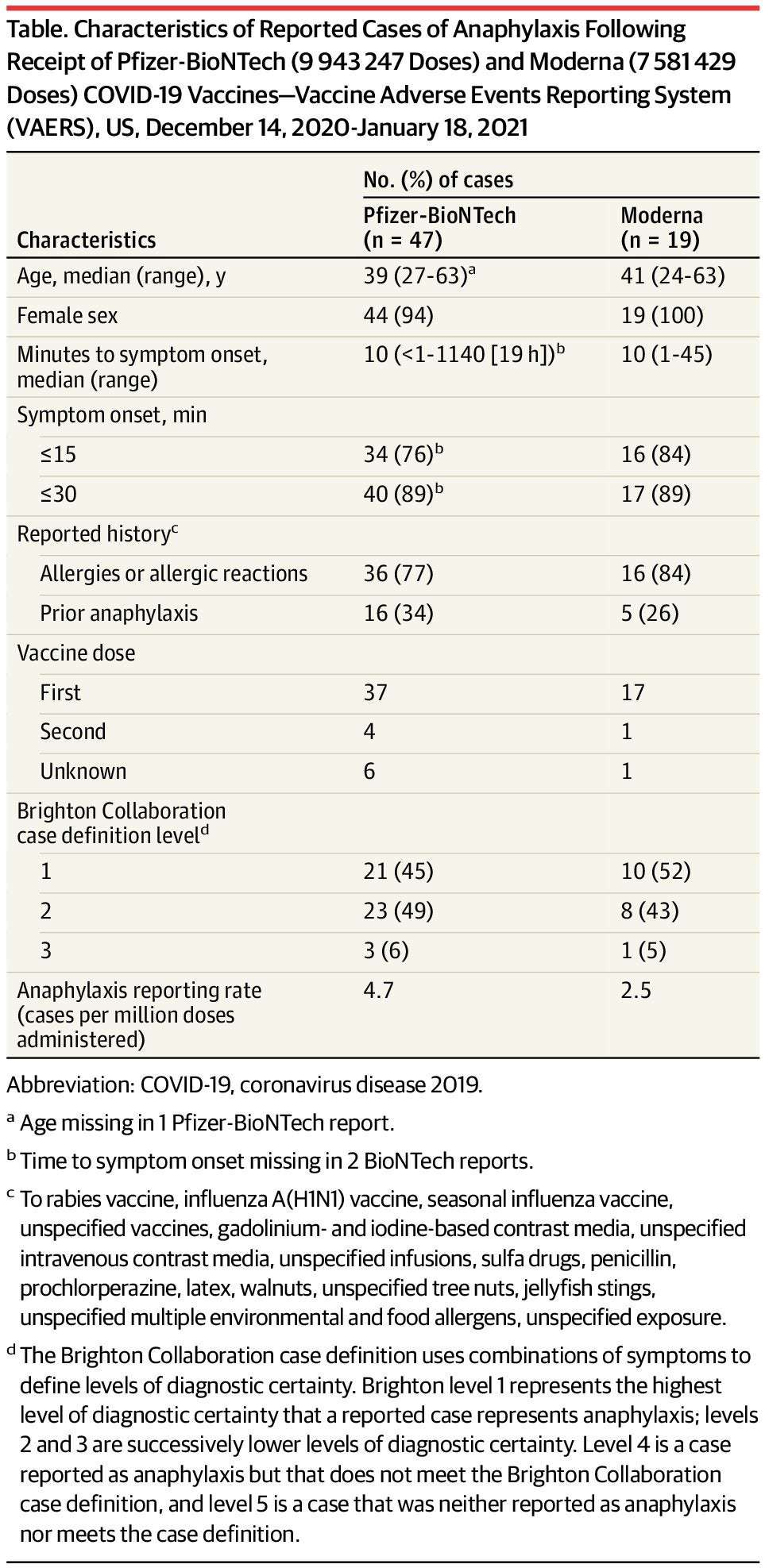
During December 14, 2020 through January 18, 2021, a total of 9 943 247 doses of the Pfizer-BioNTech vaccine and 7 581 429 doses of the Moderna vaccine were reported administered in the US (CDC unpublished data, February 2021). CDC identified 66 case reports received by VAERS that met Brighton Collaboration case definition criteria for anaphylaxis (levels 1, 2 or 3): 47 following Pfizer-BioNTech vaccine, for a reporting rate of 4.7 cases/million doses administered, and 19 following Moderna vaccine, for a reporting rate of 2.5 cases/million doses administered. Cases occurred after receipt of doses from multiple vaccine lots. Characteristics of reported cases of anaphylaxis following these vaccines are described in the Table.
Table. Characteristics of Reported Cases of Anaphylaxis Following Receipt of Pfizer-BioNTech (9 943 247 Doses) and Moderna (7 581 429 Doses) COVID-19 Vaccines—Vaccine Adverse Events Reporting System (VAERS), US, December 14, 2020-January 18, 2021
CDC physician reviewers concluded that the clinical characteristics of anaphylaxis cases following both vaccines were similar. Furthermore, there were no apparent clinical differences between anaphylaxis cases with symptom onset within 30 minutes and those with symptom onset after 30 minutes (a 15-minute postvaccination observation period is recommended for all persons and a 30-minute period is recommended for those with a history of certain allergic reactions).8 Common signs and symptoms in anaphylaxis cases were generalized urticaria, diffuse erythematous rash, angioedema, respiratory and airway obstruction symptoms, and nausea. Twenty-one (32%) of the 66 case reports noted a prior episode of anaphylaxis from other exposures; prior exposures included vaccines (rabies, influenza A[H1N1], seasonal influenza, unspecified), contrast media (gadolinium-based, iodine-based, unspecified intravenous), unspecified infusions, sulfa drugs, penicillin, prochlorperazine, latex, walnuts, unspecified tree nuts, jellyfish stings, and unspecified exposures.
In 61 (92%) of the anaphylaxis cases, patients received epinephrine as part of emergency treatment. All 66 persons were treated in health care settings; 34 (52%) were treated in an emergency department and 32 (48%) were hospitalized (including 18 in intensive care, 7 of whom required endotracheal intubation). As determined by medical record review and follow-up with treating health care facilities and clinicians, of the 7 patients who required endotracheal intubation, median time to symptom onset was 6 minutes (range, <1-45 minutes), with all but one patient having onset within 11 minutes. All 7 of those intubated received epinephrine, 6 received corticosteroids, and 5 received antihistamines; facial, tongue, or laryngeal angioedema was present in 4 of these patients; and hospitalization ranged from 1 to 3 days. Sixty-one individuals (92%) with follow-up information available are known to have been discharged from care or had recovered at the time of report to VAERS. No deaths from anaphylaxis after vaccination with either product were reported.
Continued safety monitoring of mRNA COVID-19 vaccines in the US has confirmed that anaphylaxis following vaccination is a rare event, with rates of 4.7 cases/million Pfizer-BioNTech vaccine doses administered and 2.5 cases/million Moderna vaccine doses administered, based on information through January 18, 2021. When considered in the context of morbidity and mortality from COVID-19,9 the benefits of vaccination far outweigh the risk of anaphylaxis, which is treatable. Because of the acute, life-threatening nature of anaphylaxis, immediate epinephrine administration is indicated for all cases. CDC guidance on use of mRNA COVID-19 vaccines8 and management of anaphylaxis is available.10 All facilities administering COVID-19 vaccines should have the necessary supplies and trained medical personnel available to manage anaphylaxis.
Corresponding Author: Tom Shimabukuro, MD, MPH, MBA, Immunization Safety Office, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, 1600 Clifton Rd, Atlanta, GA 30329 ([email protected]).
Published Online: February 12, 2021. doi:10.1001/jama.2021.1967
Conflict of Interest Disclosures: None reported.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC. Mention of a product or company name is for identification purposes only and does not constitute endorsement by the CDC.
Additional Contributions: We thank investigators from the CDC COVID-19 Response Team; the FDA Office of Biostatistics and Epidemiology, Center for Biologics Evaluation and Research; and the Clinical Immunization Safety Assessment Project.
shorti09 on February 13rd, 2021 at 15:07 UTC »
What do they do if you have a severe allergic reaction? Does an EpiPen work in this case?
Clackers2020 on February 13rd, 2021 at 14:25 UTC »
There's always gonna be some negative effects if the population is large enough. There's probably some people who are allergic to paracetamol. Every human body is different so we'll all react slightly differently to everything
Swarrles on February 13rd, 2021 at 13:59 UTC »
I think I'm reading this right but it looks like this has overwhelmingly only affected females? ~90% of cases for Pfizer and 100% for Moderna?
Why may that be?