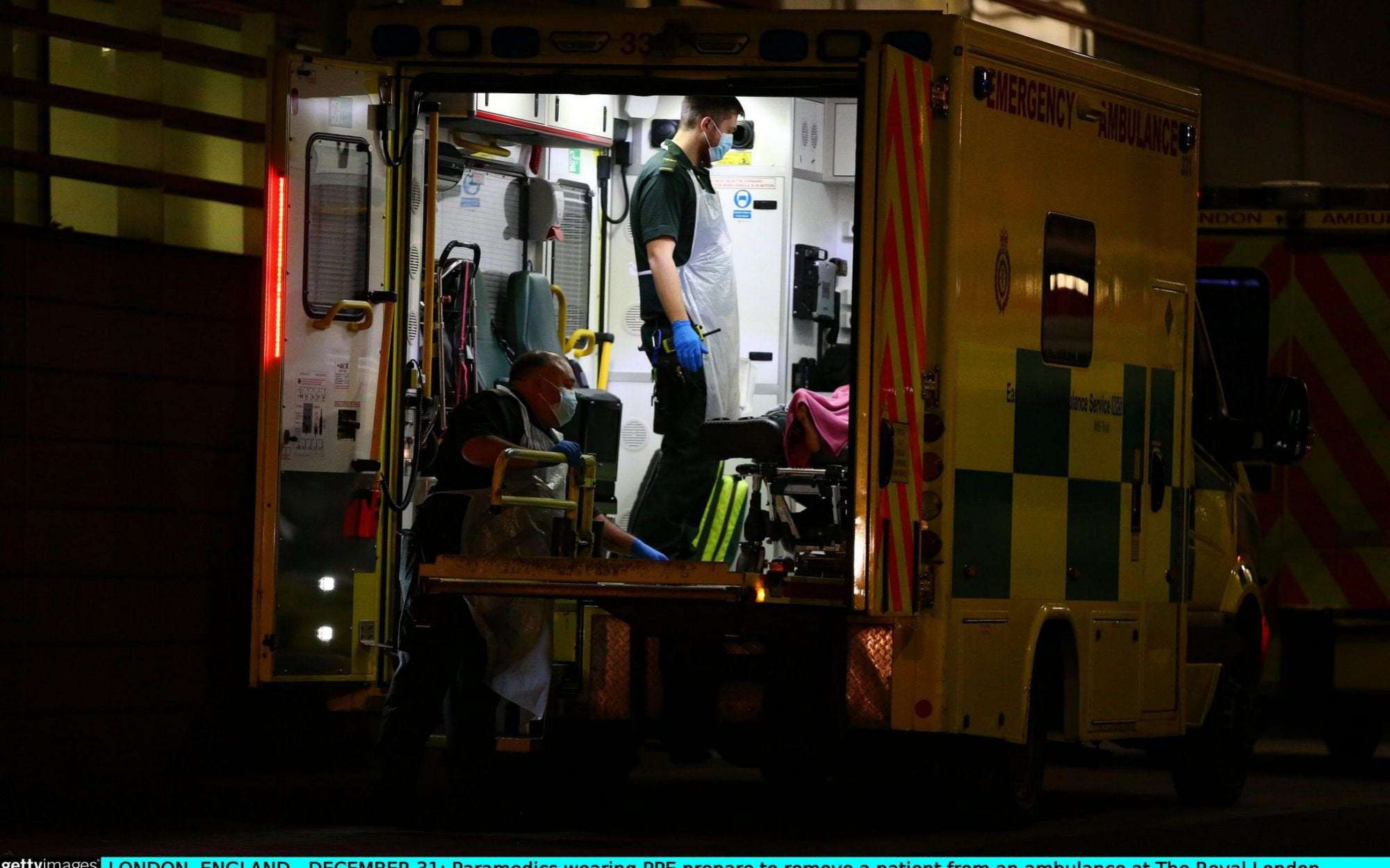
Paramedics wearing PPE prepare to remove a patient from an ambulance at The Royal London Hospital on December 31, 2020 - Hollie Adams/Getty Images Europe
Medics are starting to see “whole wards of children” suffering from Covid for the first time during the pandemic, a senior nurse has warned.
Laura Duffell, a matron at King’s College Hospital, London, said the new strain of Covid was affecting children and younger adults with no underlying health conditions in worrying numbers.
She said: “It’s very different. That’s what makes it so much scarier for us as doctors, nurses and porters and everyone else who is working on the front line.
“We have children who are coming in. It was minimally affecting children in the first wave... we now have a whole ward of children here and I know that some of my colleagues are in the same position, where they have a whole ward of children with Covid.”
Ms Duffel, a Royal College of Nursing branch official, described a picture of NHS hospitals close to buckling under the strain of rising numbers of Covid patients.
She told Radio 5 Live on Friday: “20 to 30 year olds with no underlying conditions are coming in. In intensive care you could have up to two or three very sick ventilated patients at the moment, which is far beyond what you should have.
“Some of my colleagues across London have been looking after up to 15 adults on a Covid ward with one health care assistant supporting them, so you don’t stop.”
Senior clinicians have now warned that severe staff shortages mean there is little prospect of the Nightingale hospitals riding to the rescue of the NHS as it struggles to cope with the imminent threat of being overwhelmed by Covid patients.
Consultants and nursing leaders say that high levels of nursing vacancies, coupled with high numbers of staff themselves going off sick with coronavirus or stress will make it near impossible to use the Nightingale hospitals built around the country at the start of the pandemic.
The makeshift hospitals were built at sites across England at an estimated cost of £220million, including in London, Manchester, Bristol, Sunderland, Harrogate, Exeter and Birmingham.
Of these the Exeter site received its first Covid patients in November while Manchester, Bristol and Harrogate are currently in use for non-Covid patients.
But Mike Adams, the Royal College of Nursing's England director Mike Adams said on Friday that the expectation that the Nightingale hospitals could deliver a significant increase in capacity was "misplaced".
He said: "I have real concerns that the expectation that this mass rollout in capacity can happen is misplaced because there aren't the staff to do it. If we are having to cancel leave to staff these areas, the obvious question is where will the staff come from to open the Nightingales?”
There are already one in eight nursing vacancies, with existing shortages in the type of Intensive Care Unit nurses needed to treat the most severely ill Covid patients, and recent figures showed that one in 10 Covid admissions to hospital are front line health workers - depriving the NHS of badly-needed staff.
Professor David Oliver, a trustee of the Royal College of Physicians and a senior consultant working on Covid wards, told The Telegraph: “Where are the staff going to come from for the Nightingales? The day-to day, hands-on care is carried out by nurses and health care assistants and there already aren’t enough of them.”
The warnings came as the picture across hospitals struggling to cope with a spike in Covid cases grows ever more serious, with consultants estimating that London hospitals are now operating at more than 200 per cent over capacity and even those hospitals in regions not as badly affected by the current wave working at 150 per cent over capacity.
Medics transport a patient from an ambulance to the Royal London Hospital as the spread of the coronavirus disease (COVID-19) continues - HANNAH MCKAY/Reuters
Clinicians say this means beds being placed closer together to make space, increasing the risk of cross infection between patients, and other Covid beds being moved into “every corner” of a hospital. Some major London hospitals have been forced to treat Covid-19 patients in ambulances.
As a result a growing number of non-Covid patients are having to wait longer for potentially life saving treatment for conditions such as cancer.
Department of Health data shows there were 23,813 people in hospital with Covid-19 in the UK as of December 28, the most recent figures - more than at any other point during the pandemic, even during the devastating first wave in March and April.
Some 1,847 of these patients were on ventilators in intensive care units.
There are now real fears NHS hospitals are close to being overwhelmed, with some doctors predicting this could happen when the wave of infections from the Christmas and New Year period hits them in two weeks.
Dr Shondipon Laha, a consultant in critical care medicine and honorary secretary of the Intensive Care Society, described the situation in London hospitals and some parts of the north west, as "dire".
He added: "We are close to being overwhelmed now and we will be overwhelmed soon. We are already at the limits. It's very worrying.”
Dr Laha said that patients would soon have to be transferred beyond their immediate region to areas around the country in order to create space for new admissions.
"Covid patients will soon be piling up in casualty departments because there will be nowhere else to treat them. The second peak we’re going through now in London is going to be massive. Bigger than anything we’ve ever experienced,”
“On top of that some planned operations are having to be delayed because there is no capacity at the moment to deal with them, which means people are not being treated for life threatening conditions such as cancer, including brain and stomach cancers.”
NHS England medical director Stephen Powis has described the Nightingale hospitals as "our insurance policy, there as our last resort".
TwoTreeBrain on January 2nd, 2021 at 04:51 UTC »
I watched the census on our acute care floors and ICUs go from an occasional acute Covid patient during the summer to 10-20% of all patients on any given day having Covid this last month. To be clear, we test everyone who gets admitted, and some of them are asymptomatic and are there for other reasons, but our hospital’s case rate has risen in concert with our community at large. We’ve also seen a good number of kids with the multisystem inflammatory syndrome in children associated with Covid-19 (MIS-C), and those kids are frighteningly sick. The ones with coronary artery inflammation have had it worse than any of the numerous kids with Kawasaki disease I’ve taken care of in the last 10-20 years. We don’t know what the long-term consequences of this are going to be. I’m hopeful that most if not all kids will turn out all right but that may not be the case and it will be a shame if we’ve let public policy be determined on erroneous assumptions about the impact of Covid in kids.
Edit: should clarify I work at a children’s hospital. The adult hospital across the street has been busy throughout, with ebbs and flows.
pattydickens on January 2nd, 2021 at 03:47 UTC »
We will ignore it until it becomes a gigantic fucking problem. This is the way.
Parliament_restrtoom on January 2nd, 2021 at 02:54 UTC »
People have confused "having a higher resistance to" with "being immune to" the virus.
The fact is that old people who have a more fragile health were the first victims of the virus but that young people and kids can be victims too.