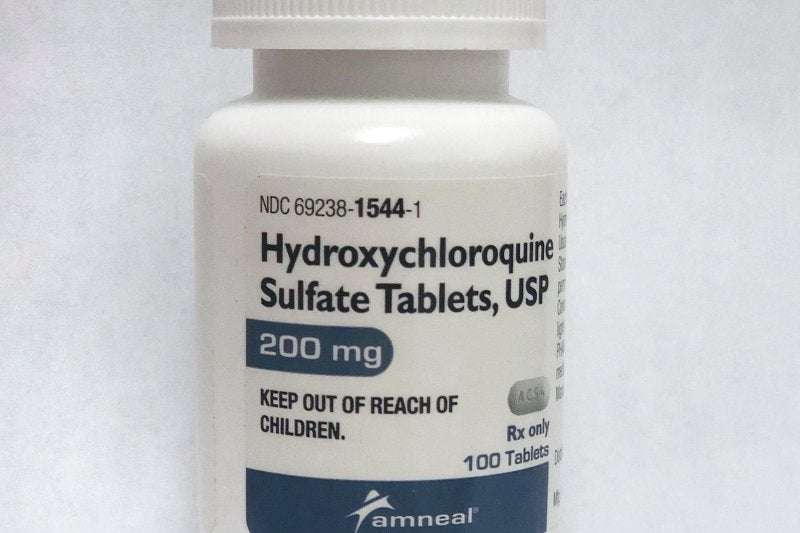
While the malaria drug hydroxychloroquine was touted early in the COVID-19 pandemic as a potential treatment, studies have found it has no effect on the infection. Photo by UPI | License Photo
Nov. 9 (UPI) -- COVID-19 patients treated with hydroxychloroquine showed no signs of significant improvement in "clinical status" compared with those given a placebo, a study published Monday by JAMA found.
Patients given a five-day course of the drug were scored as "category six" based on the World Health Organization's seven-category COVID Ordinal Outcomes Scale, the same as those given a placebo, the researchers said.
Also, 28 days after they started treatment, 10.4% of those treated with hydroxychloroquine died, just slightly lower than the 10.6% fatality rate in the placebo group.
"The results show that hydroxychloroquine did not help patients recover from COVID-19," study co-author Dr. Wesley H. Self told UPI.
"In the study, patients treated with hydroxychloroquine and those treated with a placebo had nearly identical outcomes, [so] I do not foresee any role for hydroxychloroquine in acutely ill patients hospitalized with COVID-19," said Self, an infectious disease specialist at Vanderbilt University Medical Center.
Hydroxychloroquine is an immunosuppressive and anti-parasitic drug that is used to treat malaria.
Early in the COVID-19 pandemic, it was touted by President Donald Trump and others as a potential treatment for the virus, despite the lack of any scientific data supporting its use.
Given its effectiveness helping those sickened with malaria -- a mosquito-borne infection -- to recover, "there was a strong rationale for why hydroxychloroquine may have been beneficial for patients with COVID-19," according to Self.
However, in July, the U.S. Food and Drug Administration warned against the drug's use in the treatment of those infected with the new coronavirus, due to potentially serious heart-related side effects.
For this study, Self and his colleagues treated 433 COVID-19 patients at 34 hospitals across the United States with either the drug or a placebo for a period of five days.
Patients assigned to the hydroxychloroquine group received 400 milligrams of the drug in pill form twice a day for the first two doses and then 200 mg. in pill form twice a day for the next eight doses, for a total of 10 doses over the five days.
All of the patients were then assessed based on the WHO's COVID Ordinal Outcomes Scale, which categorizes those infected according to disease severity.
Most of the patients in both the hydroxycholorquine group and the placebo group were in "category six," meaning they were hospitalized and receiving extracorporeal membrane oxygenation or invasive mechanical ventilation to maintain their breathing, the researchers said.
"Our results, especially when combined from other studies conducted in the United Kingdom and Brazil, are good evidence that hydroxychloroquine does not provide benefit for patients hospitalized with COVID-19," Self said.
mvea on November 10th, 2020 at 01:09 UTC »
For those interested, the direct link to the source journal article:
https://jamanetwork.com/journals/jama/fullarticle/2772922
Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19 A Randomized Clinical Trial
Wesley H. Self, MD, MPH1; Matthew W. Semler, MD2; Lindsay M. Leither, DO3,4; et al Jonathan D. Casey, MD, MSc2; Derek C. Angus, MD, MPH5; Roy G. Brower, MD6; Steven Y. Chang, MD, PhD7; Sean P. Collins, MD1; John C. Eppensteiner, MD8; Michael R. Filbin, MD9; D. Clark Files, MD10; Kevin W. Gibbs, MD10; Adit A. Ginde, MD, MPH11; Michelle N. Gong, MD, MS12; Frank E. Harrell Jr, PhD13; Douglas L. Hayden, PhD14; Catherine L. Hough, MD, MSc15; Nicholas J. Johnson, MD16; Akram Khan, MD15; Christopher J. Lindsell, PhD13; Michael A. Matthay, MD17; Marc Moss, MD18; Pauline K. Park, MD19; Todd W. Rice, MD2; Bryce R. H. Robinson, MD, MS20; David A. Schoenfeld, PhD14; Nathan I. Shapiro, MD, MPH21; Jay S. Steingrub, MD22; Christine A. Ulysse, MS14; Alexandra Weissman, MD, MPH23; Donald M. Yealy, MD23; B. Taylor Thompson, MD24; Samuel M. Brown, MD, MS3,4; for the National Heart, Lung, and Blood Institute PETAL Clinical Trials Network
JAMA. Published online November 9, 2020.
doi:10.1001/jama.2020.22240
Key Points
Question Does treatment with hydroxychloroquine improve clinical outcomes of adults hospitalized with coronavirus disease 2019 (COVID-19)?
Findings In this randomized clinical trial that included 479 hospitalized adults with respiratory symptoms from COVID-19, the distribution of the day 14 clinical status score (measured using a 7-category ordinal scale) was not significantly different for patients randomized to receive hydroxychloroquine compared with placebo (adjusted odds ratio, 1.02).
Meaning These findings do not support the use of hydroxychloroquine for treatment of COVID-19 among hospitalized adults.
Abstract
Importance Data on the efficacy of hydroxychloroquine for the treatment of coronavirus disease 2019 (COVID-19) are needed.
Objective To determine whether hydroxychloroquine is an efficacious treatment for adults hospitalized with COVID-19.
Design, Setting, and Participants This was a multicenter, blinded, placebo-controlled randomized trial conducted at 34 hospitals in the US. Adults hospitalized with respiratory symptoms from severe acute respiratory syndrome coronavirus 2 infection were enrolled between April 2 and June 19, 2020, with the last outcome assessment on July 17, 2020. The planned sample size was 510 patients, with interim analyses planned after every 102 patients were enrolled. The trial was stopped at the fourth interim analysis for futility with a sample size of 479 patients.
Interventions Patients were randomly assigned to hydroxychloroquine (400 mg twice daily for 2 doses, then 200 mg twice daily for 8 doses) (n = 242) or placebo (n = 237).
Main Outcomes and Measures The primary outcome was clinical status 14 days after randomization as assessed with a 7-category ordinal scale ranging from 1 (death) to 7 (discharged from the hospital and able to perform normal activities). The primary outcome was analyzed with a multivariable proportional odds model, with an adjusted odds ratio (aOR) greater than 1.0 indicating more favorable outcomes with hydroxychloroquine than placebo. The trial included 12 secondary outcomes, including 28-day mortality.
Results Among 479 patients who were randomized (median age, 57 years; 44.3% female; 37.2% Hispanic/Latinx; 23.4% Black; 20.1% in the intensive care unit; 46.8% receiving supplemental oxygen without positive pressure; 11.5% receiving noninvasive ventilation or nasal high-flow oxygen; and 6.7% receiving invasive mechanical ventilation or extracorporeal membrane oxygenation), 433 (90.4%) completed the primary outcome assessment at 14 days and the remainder had clinical status imputed. The median duration of symptoms prior to randomization was 5 days (interquartile range [IQR], 3 to 7 days). Clinical status on the ordinal outcome scale at 14 days did not significantly differ between the hydroxychloroquine and placebo groups (median [IQR] score, 6 [4-7] vs 6 [4-7]; aOR, 1.02 [95% CI, 0.73 to 1.42]). None of the 12 secondary outcomes were significantly different between groups. At 28 days after randomization, 25 of 241 patients (10.4%) in the hydroxychloroquine group and 25 of 236 (10.6%) in the placebo group had died (absolute difference, −0.2% [95% CI, −5.7% to 5.3%]; aOR, 1.07 [95% CI, 0.54 to 2.09]).
Conclusions and Relevance Among adults hospitalized with respiratory illness from COVID-19, treatment with hydroxychloroquine, compared with placebo, did not significantly improve clinical status at day 14. These findings do not support the use of hydroxychloroquine for treatment of COVID-19 among hospitalized adults.
rikkirikkiparmparm on November 10th, 2020 at 00:09 UTC »
Sort of tangential, but the other day I read that the placebo effect is apparently stronger in the U.S. than in any other country. I find that incredibly fascinating.
edit: I just looked it up again, and it's worded slightly different than what I originally said - apparently the placebo effect is growing stronger, but ONLY in the U.S..
bolivar-shagnasty on November 10th, 2020 at 00:09 UTC »
There were 433 total study participants for those who don’t want to click through.