The choir, which included 122 members, met for a 2.5-hour practice every Tuesday evening through March 10. On March 15, the choir director e-mailed the group members to inform them that on March 11 or 12 at least six members had developed fever and that two members had been tested for SARS-CoV-2 and were awaiting results. On March 16, test results for three members were positive for SARS-CoV-2 and were reported to two respective local health jurisdictions, without indication of a common source of exposure. On March 17, the choir director sent a second e-mail stating that 24 members reported that they had developed influenza-like symptoms since March 11, and at least one had received test results positive for SARS-CoV-2. The email emphasized the importance of social distancing and awareness of symptoms suggestive of COVID-19. These two emails led many members to self-isolate or quarantine before a delegated member of the choir notified SCPH on March 17.
All 122 members were interviewed by telephone either during initial investigation of the cluster (March 18–20; 115 members) or a follow-up interview (April 7–10; 117); most persons participated in both interviews. Interviews focused on attendance at practices on March 3 and March 10, as well as attendance at any other events with members during March, other potential exposures, and symptoms of COVID-19. SCPH used Council of State and Territorial Epidemiologists case definitions to classify confirmed and probable cases of COVID-19 (6). Persons who did not have symptoms at the initial interview were instructed to quarantine for 14 days from the last practice they had attended. The odds of becoming ill after attending each practice were computed to ascertain the likelihood of a point-source exposure event.
No choir member reported having had symptoms at the March 3 practice. One person at the March 10 practice had cold-like symptoms beginning March 7. This person, who had also attended the March 3 practice, had a positive laboratory result for SARS-CoV-2 by reverse transcription–polymerase chain reaction (RT-PCR) testing.
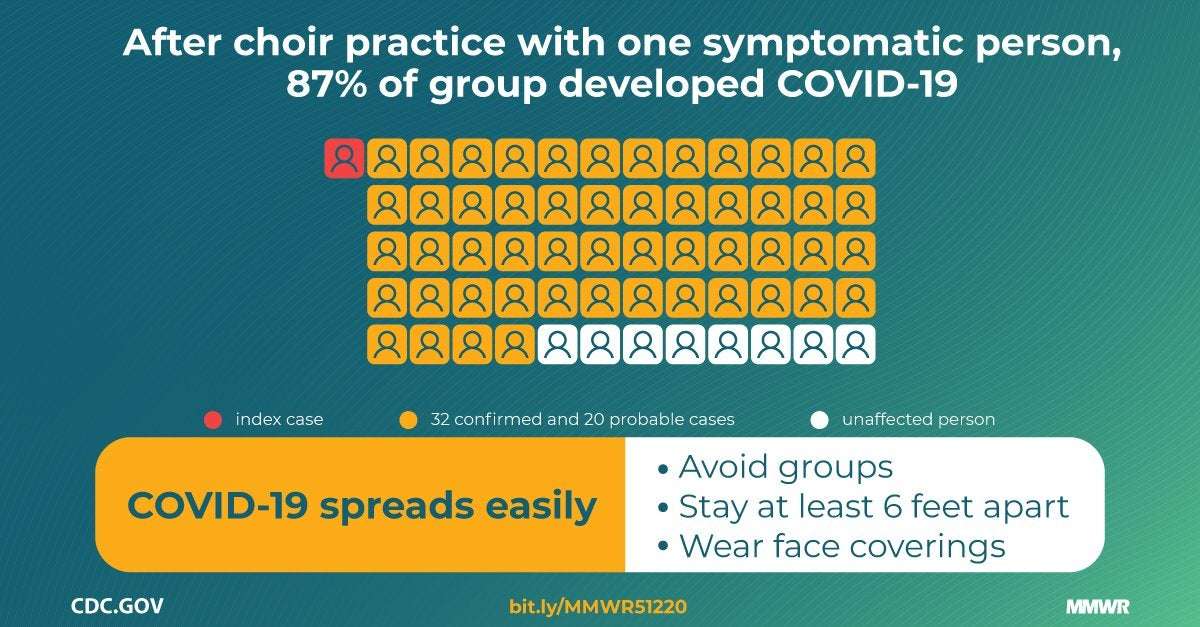
In total, 78 members attended the March 3 practice, and 61 attended the March 10 practice (Table 1). Overall, 51 (65.4%) of the March 3 practice attendees became ill; all but one of these persons also attended the March 10 practice. Among 60 attendees at the March 10 practice (excluding the patient who became ill March 7, who also attended), 52 (86.7%) choir members subsequently became ill. Some members exclusively attended one practice; among 21 members who only attended March 3, one became ill and was not tested (4.8%), and among three members who only attended March 10, two became ill (66.7%), with one COVID-19 case being laboratory-confirmed.
Because illness onset for 49 (92.5%) patients began during March 11–15 (Figure), a point-source exposure event seemed likely. The median interval from the March 3 practice to symptom onset was 10 days (range = 4–19 days), and from the March 10 practice to symptom onset was 3 days (range = 1–12 days). The odds of becoming ill after the March 3 practice were 17.0 times higher for practice attendees than for those who did not attend (95% confidence interval [CI] = 5.5–52.8), and after the March 10 practice, the odds were 125.7 times greater (95% CI = 31.7–498.9). The clustering of symptom onsets, odds of becoming ill according to practice attendance, and known presence of a symptomatic contagious case at the March 10 practice strongly suggest that date as the more likely point-source exposure event. Therefore, that practice was the focus of the rest of the investigation. Probable cases were defined as persons who attended the March 10 practice and developed clinically compatible COVID-19 symptoms, as defined by Council of State and Territorial Epidemiologists (6). The choir member who was ill beginning March 7 was considered the index patient.
The March 10 choir rehearsal lasted from 6:30 to 9:00 p.m. Several members arrived early to set up chairs in a large multipurpose room. Chairs were arranged in six rows of 20 chairs each, spaced 6–10 inches apart with a center aisle dividing left and right stages. Most choir members sat in their usual rehearsal seats. Sixty-one of the 122 members attended that evening, leaving some members sitting next to empty seats. Attendees practiced together for 40 minutes, then split into two smaller groups for an additional 50-minute practice, with one of the groups moving to a smaller room. At that time, members in the larger room moved to seats next to one another, and members in the smaller room sat next to one another on benches. Attendees then had a 15-minute break, during which cookies and oranges were available at the back of the large room, although many members reported not eating the snacks. The group then reconvened for a final 45-minute session in their original seats. At the end of practice, each member returned their own chair, and in the process congregated around the chair racks. Most attendees left the practice immediately after it concluded. No one reported physical contact between attendees. SCPH assembled a seating chart of the all-choir portion of the March 10 practice (not reported here because of concerns about patient privacy).
Among the 61 choir members who attended the March 10 practice, the median age was 69 years (range = 31–83 years); 84% were women. Median age of those who became ill was 69 years, and 85% of cases occurred in women. Excluding the laboratory-confirmed index patient, 52 (86.7%) of 60 attendees became ill; 32 (61.5%) of these cases were confirmed by RT-PCR testing and 20 (38.5%) persons were considered to have probable infections. These figures correspond to secondary attack rates of 53.3% and 86.7% among confirmed and all cases, respectively. Attendees developed symptoms 1 to 12 days after the practice (median = 3 days). The first SARS-CoV-2 test was performed on March 13. The last person was tested on March 26.
Three of the 53 patients were hospitalized (5.7%), including two who died (3.8%). The mean interval from illness onset to hospitalization was 12 days. The intervals from onset to death were 14 and 15 days for the two patients who died.
SCPH collected information about patient signs and symptoms from patient interviews and hospital records (Table 2). Among persons with confirmed infections, the most common signs and symptoms reported at illness onset and at any time during the course of illness were cough (54.5% and 90.9%, respectively), fever (45.5%, 75.8%), myalgia (27.3%, 75.0%), and headache (21.2%, 60.6%). Several patients later developed gastrointestinal symptoms, including diarrhea (18.8%), nausea (9.4%), and abdominal cramps or pain (6.3%). One person experienced only loss of smell and taste. The most severe complications reported were viral pneumonia (18.2%) and severe hypoxemic respiratory failure (9.1%).
Among the recognized risk factors for severe illness, the most common was age, with 75.5% of patients aged ≥65 years. Most patients (67.9%) did not report any underlying medical conditions, 9.4% had one underlying medical condition, and 22.6% had two or more underlying medical conditions. All three hospitalized patients had two or more underlying medical conditions.
newleafkratom on May 12nd, 2020 at 23:42 UTC »
The reason so many singers seem to be susceptible: “Certain persons, known as superemitters, who release more aerosol particles during speech than do their peers, might have contributed to this and previously reported COVID-19 superspreading events”
Icedcoffeeee on May 12nd, 2020 at 20:50 UTC »
This is important. I've noticed a lot of the language around reopening talks about frequent cleaning. Cleaning won't help most transmissions. There's another article Ive seen that shows infection in a similar way at several restaurant tables.
molten_dragon on May 12nd, 2020 at 17:18 UTC »
I would imagine choir practice would be about the worst case scenario for respiratory transmission of a virus.